
The Glymphatic System: How Poor Sleep ‘Clogs’ Your Brain (And How to Fix It)
Introduction
Imagine your brain as a high-performance engine. Just like an engine needs oil changes to run smoothly, your brain requires a nightly “cleaning cycle” to flush out toxins, dead cells, and harmful proteins. This process is managed by the glymphatic system—a recently discovered waste-clearance network that works primarily during deep sleep.
But what happens when you don’t get enough sleep? Research shows that poor sleep “clogs” your brain, allowing toxic debris like beta-amyloid (linked to Alzheimer’s) to accumulate. Over time, this can impair memory, focus, and even long-term brain health.
In this article, you’ll learn:
✔ What the glymphatic system is (and why it’s crucial for brain health)
✔ How sleep deprivation disrupts this cleaning process
✔ 5 science-backed ways to “unclog” your brain and optimize glymphatic flow
What Is the Glymphatic System?

Discovered in 2012 by neuroscientist Dr. Maiken Nedergaard, the glymphatic system is the brain’s waste-removal system. It’s named after the glial cells that support it and the lymphatic-like function it performs.
How It Works
- Cerebrospinal fluid (CSF) flows through brain tissues.
- It washes away metabolic waste (beta-amyloid, tau proteins, dead cells).
- Waste is drained into the body’s lymphatic system for disposal.
Key Fact: The glymphatic system is 10x more active during deep sleep (non-REM stages) than when awake.
How Poor Sleep “Clogs” Your Brain
When you skimp on sleep, the glymphatic system can’t perform its nightly detox, leading to:
1. Toxic Buildup in the Brain
- Beta-amyloid plaques (associated with Alzheimer’s) accumulate.
- Tau proteins (linked to neurodegeneration) clump together.
- Inflammatory cytokines increase, raising the risk of brain fog and depression.
Study Alert: A 2023 Nature study found that just one night of poor sleep increases beta-amyloid levels by 5-10%.
2. Slower Cognitive Function
- Reduced memory consolidation (sleep is when memories solidify).
- Impaired focus and decision-making (due to “dirty” neural pathways).
- Increased brain fog and mental fatigue.
3. Higher Risk of Neurological Disorders
Chronic sleep deprivation is linked to:
- Alzheimer’s disease
- Parkinson’s disease
- Multiple sclerosis (MS)
5 Ways to Boost Glymphatic Flow (and “Unclog” Your Brain)

1. Prioritize Deep Sleep
The glymphatic system works best during slow-wave sleep (Stage 3 non-REM).
How to get more deep sleep:
- Keep a consistent sleep schedule (even on weekends).
- Sleep in a cool room (60-67°F)—cool temps enhance deep sleep.
- Avoid alcohol before bed—it disrupts sleep architecture.
2. Sleep on Your Side
Research suggests the lateral (side) sleeping position may optimize glymphatic drainage compared to back or stomach sleeping.
Why? It improves CSF flow and reduces brain compression.
3. Exercise Regularly (But Time It Right)
- Aerobic exercise (walking, jogging, cycling) increases CSF circulation.
- Yoga and stretching improve lymphatic drainage.
Timing Tip: Avoid intense workouts within 3 hours of bedtime—they can raise cortisol and disrupt sleep.
4. Eat a Brain-Cleansing Diet
Certain foods support glymphatic function:
- Omega-3s (fatty fish, walnuts) – Reduce brain inflammation.
- Turmeric/curcumin – Lowers beta-amyloid buildup.
- Leafy greens (kale, spinach) – High in folate, which aids detox.
Avoid: Excess sugar and processed foods (they increase brain inflammation).
5. Try Intermittent Fasting (or Time-Restricted Eating)
Fasting for 12-16 hours overnight (e.g., eating dinner by 7 PM, breakfast at 7 AM) may:
- Enhance autophagy (cellular cleanup).
- Improve CSF turnover.
Bonus: Hydrate well—dehydration thickens CSF, slowing waste removal.
The Bottom Line
Your brain’s glymphatic system is its self-cleaning mechanism, and sleep is the “on” switch. Neglecting sleep doesn’t just make you tired—it leaves toxic waste lingering in your brain, increasing the risk of cognitive decline.
Action Steps Tonight:
- Go to bed 30 minutes earlier to maximize deep sleep.
- Sleep on your side if possible.
- Hydrate well (but reduce liquids 1-2 hours before bed to avoid waking up).
Long-Term Fix: Make sleep a non-negotiable pillar of health—your future brain will thank you.

High-Functioning Anxiety: Signs You Might Have It (Even If You Seem Fine)
Introduction
High-Functioning Anxiety, When people think of anxiety, they often picture someone visibly panicking, avoiding social situations, or struggling to function. But what if you appear completely “fine” on the outside—successful, productive, and put-together—while battling constant inner turmoil?
This is high-functioning anxiety (HFA): a hidden struggle where individuals maintain their daily responsibilities but experience relentless worry, perfectionism, and mental exhaustion. Unlike generalized anxiety disorder (GAD), HFA isn’t an official diagnosis, but it’s a real and exhausting experience for millions.
In this article, we’ll explore:
✔ What high-functioning anxiety really is
✔ Subtle signs you might have it (even if no one notices)
✔ Why it often goes undiagnosed
✔ How to manage it before burnout hits
What Is High-Functioning Anxiety?
High-functioning anxiety isn’t listed in the DSM-5 (the manual for mental health diagnoses), but therapists recognize it as a subset of anxiety where individuals cope well externally while suffering internally.
People with HFA are often:
✅ High achievers (overachievers, even)
✅ Meticulous planners
✅ Seen as “reliable” or “the strong one”
✅ Always busy (to avoid quiet moments with their thoughts)
Yet beneath the surface, they deal with:
🔴 Chronic overthinking
🔴 Fear of failure (despite success)
🔴 Physical symptoms (insomnia, digestive issues, muscle tension)
🔴 Difficulty relaxing
Unlike classic anxiety disorders, HFA doesn’t always interfere with daily life—it fuels it. But this can lead to burnout, health problems, and emotional breakdowns over time.
9 Hidden Signs of High-Functioning Anxiety

1. You’re a Perfectionist (to a Fault)
- You redo tasks obsessively, even when they’re “good enough.”
- Mistakes feel catastrophic, even minor ones.
- You procrastinate because starting means facing potential failure.
Example: Spending hours editing an email that only needed a quick reply.
2. You Overprepare for Everything
- You rehearse conversations in your head before they happen.
- You arrive excessively early to appointments “just in case.”
- You mentally plan escape routes from social events.
Why? Your brain tries to control outcomes to avoid discomfort.
3. You Say “Yes” to Everything (Then Regret It)
People with HFA often:
- Agree to extra work to prove their worth.
- Fear disappointing others.
- End up overwhelmed but hide it.
Result: Exhaustion from overcommitment.
4. You’re Mentally Exhausted but Can’t Relax
- Even during downtime, your brain races with “what-ifs.”
- You feel guilty for resting (“I should be doing something productive”).
- Hobbies feel stressful if you’re not “good” at them.
5. You Ruminate on Past Conversations
- Overanalyzing interactions: “Did I sound stupid?”
- Fixating on minor criticisms for days.
- Assuming others judge you harsher than they do.
6. Physical Symptoms You Ignore
HFA often manifests physically as:
- Insomnia or restless sleep
- Jaw clenching/teeth grinding (bruxism)
- Stomach issues (IBS, nausea)
- Frequent headaches or muscle tension
Why? Chronic anxiety keeps the body in “fight or flight” mode.
7. You Use Busyness as a Distraction
- Always filling silence with podcasts, chores, or work.
- Fear of stillness (because quiet = intrusive thoughts).
- Feeling uneasy with unstructured time.
8. You Downplay Your Anxiety
- “I’m fine—I just care a lot!”
- Masking stress with humor or overworking.
- Avoiding therapy because “it’s not that bad.”
9. You Fear Success as Much as Failure
- Self-sabotage when things go well (“What if I can’t keep this up?”).
- Imposter syndrome, even with accomplishments.
- Waiting for the “other shoe to drop” in good times.
Why High-Functioning Anxiety Goes Undiagnosed

- It’s Misunderstood: Since sufferers appear competent, their struggle is dismissed as “just being diligent.”
- No “Obvious” Breakdowns: They don’t miss work or social events, so others don’t see the cost.
- Self-Medicating: Some use caffeine, alcohol, or overwork to cope, masking symptoms.
- Stigma: Admitting anxiety feels like admitting weakness, especially in high-achievers.
The Danger: Untreated HFA can lead to:
- Burnout
- Depression
- Chronic health issues (heart disease, autoimmune disorders)
How to Manage High-Functioning Anxiety
1. Name It to Tame It
Acknowledge your anxiety instead of justifying it as “just how I am.” Journaling prompts:
- “What am I afraid will happen if I slow down?”
- “When did I first feel this pressure to be perfect?”
2. Set Boundaries (Start Small)
- Practice saying “Let me think about it” before agreeing to requests.
- Schedule “nothing” time (yes, it counts as productivity).
3. Embrace “Good Enough”
- Try the 80% rule: If a task is 80% done, it’s complete.
- Ask: “Will this matter in 5 years?”
4. Rewire Your Nervous System
- Diaphragmatic breathing (5-second inhale, 7-second exhale).
- Progressive muscle relaxation (tense/release each muscle group).
- Cold showers (resets the vagus nerve, reducing panic signals).
5. Challenge Catastrophic Thoughts
For “What if I fail?” ask:
- “What’s the actual worst-case scenario?”
- “How would I handle it?”
6. Seek Professional Help
Therapy options:
- CBT (Cognitive Behavioral Therapy): Identifies and reframes anxious thought patterns.
- Acceptance and Commitment Therapy (ACT): Teaches mindfulness alongside action.
- Medication (if needed): SSRIs can help regulate chemical imbalances.
Final Thoughts
High-functioning anxiety is a silent struggle, but it doesn’t have to be permanent. Whether the goal isn’t to eliminate anxiety entirely—it’s to prevent it from stealing your joy and health.
If you saw yourself in these signs:
🔹 You’re not “just Type A.”
🔹 You don’t have to white-knuckle through life.
🔹 Small changes today prevent bigger crashes tomorrow.
Next Step: Try one anxiety-reducing tactic this week (e.g., 5 minutes of deep breathing daily). Progress over perfection.

How Depression Affects Relationships: Tips for Partners and Loved Ones
📝 Introduction
Depression is a mental health condition that affects millions of people worldwide. However, its impact goes far beyond the individual—it also profoundly influences relationships with partners, family members, and friends. When someone you care about is struggling with depression, it can create emotional distance, communication challenges, and feelings of helplessness.
In this article, we’ll explore how depression affects relationships, offer practical tips for supporting loved ones, and share strategies for maintaining emotional intimacy while prioritizing self-care.
🌫️ Understanding Depression in Relationships

Depression is more than just sadness—it is a persistent mental health condition that affects mood, energy levels, and behavior. When depression enters a relationship, it can create unique challenges, including:
- Emotional withdrawal: The person with depression may become emotionally distant or unresponsive.
- Communication breakdown: Depression can make it difficult to express emotions or engage in meaningful conversations.
- Changes in intimacy: Reduced interest in physical affection or intimacy is common.
- Feelings of guilt or frustration: Both partners may experience feelings of guilt, inadequacy, or resentment.
Recognizing these patterns is the first step toward navigating the challenges together.
💔 The Impact of Depression on Romantic Relationships
1. Emotional Distance and Disconnection
Depression can cause emotional numbness, making it hard for the affected individual to express love, affection, or empathy. Partners may feel rejected or unloved, even though it is the depression—not the person—causing this behavior.
💡 Tip: Practice patience and compassion. Remind yourself that the emotional withdrawal is not personal.
2. Decreased Physical Intimacy
Depression often reduces libido and physical affection, leading to a lack of intimacy. This can cause confusion or feelings of rejection in the unaffected partner.
💡 Tip: Openly discuss intimacy challenges without blame. Prioritize emotional connection before physical intimacy by spending quality time together.
3. Increased Irritability or Conflict
Individuals with depression may become more irritable or easily frustrated, leading to frequent misunderstandings or arguments.
💡 Tip: Practice active listening during conflicts. Avoid personalizing mood changes, and recognize when to take a step back to prevent escalation.
👨👩👧👦 Depression’s Effect on Family Relationships

Depression doesn’t only affect romantic partners—it can also strain family dynamics.
- Parents and Children: A parent’s depression can lead to emotional unavailability, affecting children’s emotional well-being. Conversely, caring for a depressed parent can be overwhelming for children.
- Siblings or Extended Family: Depression may create feelings of helplessness or guilt among family members, who may not know how to provide support.
💡 Tips for Families:
- Educate yourself: Learn about depression to better understand what your loved one is going through.
- Encourage family therapy: Family counseling can help improve communication and reduce tension.
- Foster open dialogue: Create a safe space for honest conversations about mental health without judgment.
💕 How Depression Affects Friendships
Depression can also strain friendships. People with depression may withdraw from social activities, ignore messages, or cancel plans. Friends may interpret this as disinterest or rejection, leading to strained or distant friendships.
💡 Tips for Supporting a Friend with Depression:
- Stay in touch: Even if they seem distant, send a simple message to let them know you’re there.
- Be patient with cancellations: People with depression often have low energy. Don’t take frequent cancellations personally.
- Offer specific support: Instead of saying, “Let me know if you need anything,” offer concrete help, like bringing over a meal or going for a walk.
🌿 Tips for Supporting a Partner or Loved One with Depression
Supporting someone with depression can be emotionally challenging. Here are effective strategies to help:
✅ 1. Learn About Depression
Educate yourself about depression symptoms, causes, and treatment options. Understanding that depression is a mental health condition, not a choice, helps reduce frustration and fosters compassionate support.
💡 Tip: Use reliable sources like mental health websites or books to learn about depression.
✅ 2. Maintain Open Communication
Honest and empathetic communication is essential in relationships affected by depression.
- Use “I” statements: Instead of saying, “You never talk to me anymore,” say, “I miss spending time with you.”
- Validate their feelings: Acknowledge their pain rather than dismissing it with statements like, “You’ll get over it.”
✅ 3. Encourage Professional Help
While support from loved ones is vital, professional treatment is often necessary for managing depression.
- Encourage therapy or counseling: Suggest seeking help from a mental health professional.
- Support medication management: If applicable, remind them to follow their prescribed treatment plan.
💡 Tip: Offer to help find a therapist or accompany them to their first appointment if they feel anxious.
✅ 4. Set Healthy Boundaries
Supporting someone with depression doesn’t mean sacrificing your own mental health.
- Define emotional boundaries: It’s okay to step back when needed to recharge.
- Avoid enabling behaviors: Don’t shield them from consequences of harmful actions, but offer gentle support.
💡 Tip: Prioritize self-care by engaging in activities that bring you peace and joy.
✅ 5. Celebrate Small Wins
Depression recovery is gradual, and small steps matter.
- Acknowledge progress: Celebrate small achievements, such as attending therapy or getting out of bed.
- Offer positive reinforcement: Praise their efforts and show appreciation for their resilience.
💙 Self-Care for Partners and Loved Ones
Supporting someone with depression can be emotionally taxing. Prioritize your own mental health by:
- Practicing self-care: Engage in activities that recharge you, such as yoga, hobbies, or time with friends.
- Seeking support: Join support groups for caregivers or talk to a mental health professional.
- Avoiding burnout: Set realistic expectations and remember that you can’t “fix” someone’s depression.
🌟 When to Seek Professional Help as a Couple or Family
If depression is severely impacting your relationship, consider couples or family therapy.
- Therapy helps you improve communication and learn coping strategies.
- A mental health professional can provide guidance on navigating challenges as a team.
✅ Conclusion
Depression can significantly affect romantic relationships, friendships, and family bonds, but with understanding, patience, and support, relationships can remain strong and even grow deeper.
By practicing compassionate communication, encouraging professional help, and prioritizing self-care, you can effectively support your loved one while safeguarding your own well-being.
❤️ Remember: You are not alone—help and support are available for both individuals with depression and their loved ones.

PTSD vs. CPTSD: Understanding the Key Differences and Symptoms
📝 Introduction
Post-Traumatic Stress Disorder (PTSD) and Complex Post-Traumatic Stress Disorder (CPTSD) are mental health conditions triggered by traumatic events. While they share overlapping symptoms, they are distinct disorders with different causes, manifestations, and treatments.
In this blog post, we’ll explore:
- The definitions and causes of PTSD and CPTSD
- Their symptoms and diagnostic differences
- Treatment options for each condition
- How to support someone with PTSD or CPTSD
🌿 What is PTSD?

Post-Traumatic Stress Disorder (PTSD) is a psychiatric condition that occurs after exposure to a traumatic event. It can develop following experiences such as:
- Combat or war exposure (common in veterans)
- Serious accidents (car crashes, natural disasters)
- Physical or sexual assault
- Sudden loss of a loved one
- Witnessing violence
✅ Symptoms of PTSD
The symptoms of PTSD typically fall into four categories:
- Re-experiencing symptoms:
- Flashbacks, reliving the trauma
- Distressing memories or nightmares
- Emotional or physical reactions to trauma reminders
- Avoidance symptoms:
- Avoiding people, places, or activities that trigger memories
- Emotional numbness or detachment
- Negative changes in mood and thoughts:
- Persistent negative thoughts or beliefs
- Guilt, shame, or blame
- Difficulty remembering details of the event
- Arousal and reactivity symptoms:
- Irritability or anger outbursts
- Hypervigilance or being easily startled
- Sleep disturbances or insomnia
🌿 What is CPTSD?

Complex Post-Traumatic Stress Disorder (CPTSD) is a more severe form of PTSD that arises from prolonged or repeated trauma over an extended period. Unlike PTSD, which may result from a single traumatic event, CPTSD develops from chronic trauma such as:
- Childhood abuse or neglect
- Ongoing domestic violence
- Human trafficking or slavery
- Repeated exposure to violence or war
✅ Symptoms of CPTSD
In addition to the core symptoms of PTSD, individuals with CPTSD experience three additional symptoms:
- Emotional dysregulation:
- Persistent sadness, depression, or mood swings
- Difficulty controlling anger or emotional outbursts
- Negative self-concept:
- Chronic feelings of worthlessness, guilt, or shame
- Deep-rooted beliefs of being damaged or unlovable
- Interpersonal difficulties:
- Trouble forming or maintaining relationships
- Trust issues and social withdrawal
- Fear of abandonment or rejection
🔥 Key Differences Between PTSD and CPTSD
While PTSD and CPTSD share similarities, there are distinct differences in their:
| Aspect | PTSD | CPTSD |
|---|---|---|
| Cause | Single traumatic event | Repeated or prolonged trauma |
| Symptoms | Flashbacks, avoidance, hypervigilance | Emotional dysregulation, low self-worth, relational difficulties |
| Emotional Impact | Fear-based reactions | Chronic emotional numbness and instability |
| Relationships | May avoid certain relationships | Struggles with trust and intimacy |
| Treatment Needs | Trauma-focused therapy | Trauma-focused + emotional regulation therapies |
💡 PTSD vs. CPTSD: Diagnosing the Disorders
Both PTSD and CPTSD can be diagnosed by mental health professionals using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases (ICD-11).
- PTSD is officially recognized in the DSM-5 with clear diagnostic criteria.
- CPTSD is included in the ICD-11 but not yet classified as a separate disorder in the DSM-5.
Diagnosis involves:
- Clinical interviews: Reviewing trauma history and symptoms.
- Standardized assessments: Tools like the PTSD Checklist (PCL) or the ICD-11 CPTSD Checklist.
- Symptom duration: PTSD symptoms must persist for at least one month to qualify for diagnosis.
🌿 Treatment Options for PTSD and CPTSD
Effective treatment approaches vary slightly for PTSD and CPTSD due to the different symptom profiles.
✅ Treatment for PTSD
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
- Aims to restructure negative thought patterns.
- Helps reduce avoidance behaviors and flashbacks.
- Eye Movement Desensitization and Reprocessing (EMDR)
- Uses bilateral stimulation (eye movements) to help reprocess traumatic memories.
- Medications
- SSRIs or SNRIs (e.g., sertraline, paroxetine) to reduce anxiety and depression.
- Prazosin for trauma-related nightmares.
✅ Treatment for CPTSD
- Dialectical Behavior Therapy (DBT)
- Effective for emotional regulation and reducing impulsivity.
- Includes mindfulness and distress tolerance techniques.
- Schema Therapy
- Helps address deep-seated beliefs of self-worthlessness.
- Focuses on rebuilding a healthier self-image.
- Medications
- Antidepressants or mood stabilizers to manage mood swings and depression.
- Adjunctive therapies (such as trauma-informed yoga) for emotional regulation.
💕 How to Support Someone with PTSD or CPTSD
Supporting a loved one with PTSD or CPTSD requires empathy, patience, and understanding.
✅ Ways to Help:
- Educate yourself: Learn about the conditions to reduce stigma and increase empathy.
- Listen without judgment: Allow them to share their feelings at their own pace.
- Encourage professional help: Suggest seeking therapy or counseling.
- Respect their boundaries: Avoid pushing them to discuss traumatic experiences.
- Help with triggers: Assist in identifying and minimizing trauma triggers.
🎯 Conclusion
While PTSD and CPTSD share similarities, they are distinct disorders with unique symptom profiles and treatment needs.
- PTSD often results from a single traumatic event, while CPTSD develops from chronic, repeated trauma.
- Both conditions benefit from trauma-informed therapy and support from loved ones.
- If you or someone you know is struggling with PTSD or CPTSD, seeking professional help is the first step toward healing.

Understanding Postpartum Depression: Symptoms and Treatment Options
Postpartum depression (PPD) is a serious mental health condition that affects many new mothers after childbirth. While it is normal for mothers to experience some mood changes during the postpartum period due to hormonal fluctuations, PPD is much more than the “baby blues.” It can interfere with daily life and pose significant challenges for new parents. Understanding the symptoms of postpartum depression, its causes, and treatment options is essential for anyone affected by it or supporting someone who is. In this comprehensive blog post, we will explore postpartum depression in detail, from symptoms to treatment, and how to seek help.
What is Postpartum Depression?
Postpartum depression is a type of depression that occurs after childbirth. Unlike the mild mood swings often experienced during the early days after having a baby (known as the “baby blues”), postpartum depression is more severe and persistent. It can begin within the first few weeks after delivery, but it can also develop up to a year after childbirth. PPD affects not only the mother but can also influence the entire family, including the newborn.
Symptoms of Postpartum Depression

The symptoms of postpartum depression can vary from mild to severe, and they can interfere with a mother’s ability to care for herself and her baby. Some of the most common signs and symptoms include:
- Intense Feelings of Sadness or Hopelessness
A new mother may feel overwhelmed by sadness or despair, often with no clear reason. These feelings can be accompanied by a sense of hopelessness or that things will never improve. - Difficulty Bonding with the Baby
Mothers with PPD may struggle to bond with their newborn, feeling disconnected or detached from the baby. This can lead to feelings of guilt and inadequacy as a mother. - Fatigue and Exhaustion
While it’s normal to feel tired after childbirth, the fatigue associated with PPD is more intense. Even after getting adequate rest, new mothers may feel drained and unable to function. - Loss of Interest in Activities
A mother with postpartum depression may lose interest in activities that she once enjoyed. This lack of enthusiasm can also extend to caring for herself, eating, or engaging in social activities. - Anxiety or Panic Attacks
Along with feelings of sadness, anxiety often accompanies postpartum depression. Mothers may feel constant worry, and panic attacks can occur without warning. - Changes in Appetite or Sleep Patterns
Some mothers may experience a loss of appetite, while others may eat excessively. Changes in sleep patterns, such as insomnia or sleeping too much, are also common symptoms of PPD. - Thoughts of Harm or Self-Harm
In severe cases, a mother with postpartum depression may have thoughts of harming herself or her baby. If this occurs, it is crucial to seek professional help immediately. - Irritability or Anger
PPD can lead to feelings of irritability and frustration, and mothers may become easily agitated or angry, even at small things. - Guilt or Shame
Many mothers with postpartum depression experience intense guilt, feeling that they are not living up to expectations or being “good” mothers. This can exacerbate feelings of isolation.
Causes of Postpartum Depression

The exact cause of postpartum depression is not fullY understood, but it is believed to result from a combination of physical, emotional, and environmental factors. Here are some potential contributors to PPD:
- Hormonal Changes
After childbirth, a woman’s hormone levels, particularly estrogen and progesterone, drop significantly. These hormonal shifts can lead to mood swings and contribute to the development of depression. - Physical Changes
Pregnancy and childbirth bring significant physical changes to the body. Exhaustion from labor, changes in weight, and physical recovery can affect a woman’s mental health and increase the risk of depression. - Sleep Deprivation
New mothers often experience sleep deprivation due to nighttime feedings, baby care, and adjusting to a new routine. Chronic sleep deprivation is linked to mood disorders like depression. - Emotional Factors
The transition to motherhood can be emotionally overwhelming. First-time mothers may feel unprepared or unsure of their parenting abilities. Additionally, previous history of depression or anxiety can increase the risk of postpartum depression. - Stress and Life Circumstances
Financial stress, lack of social support, or relationship difficulties can contribute to postpartum depression. Women who experience difficult pregnancies, complications during childbirth, or a lack of help from their partner or family may be more prone to PPD. - Previous Mental Health History
Women with a history of depression or anxiety, either during pregnancy or in the past, are more likely to experience postpartum depression. A personal or family history of mental illness can increase the risk.
Treatment Options for Postpartum Depression
Postpartum depression is treatable, and there are several treatment options available to help mothers recover. It is essential to seek professional help if you suspect that you have PPD. Here are some of the most common treatment options:
1. Therapy and Counseling
Cognitive Behavioral Therapy (CBT) and other forms of psychotherapy can be very effective in treating postpartum depression. Therapy can help new mothers address negative thought patterns, manage emotions, and develop healthier coping strategies. A therapist will work with the mother to explore underlying emotional issues and provide tools to manage stress and improve mental well-being.
2. Medications
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are often prescribed to women with moderate to severe postpartum depression. These medications help balance brain chemicals associated with mood regulation. It is important to discuss the benefits and potential risks of medication with a healthcare provider, especially if breastfeeding, as some medications can be passed to the baby through breast milk.
3. Support Groups
Joining a support group can provide a sense of community for new mothers struggling with postpartum depression. Sharing experiences and connecting with others who understand can be incredibly validating. Support groups are often led by trained professionals and can help reduce feelings of isolation.
4. Lifestyle Changes and Self-Care
Incorporating self-care practices into daily life is vital for mental health recovery. This includes getting adequate rest, eating a balanced diet, engaging in light physical activity, and taking time for relaxation and hobbies. It’s essential for new mothers to ask for help from family members or partners, take breaks, and not feel guilty about needing time for themselves.
5. Partner and Family Support
Having a supportive partner and family is crucial for the recovery process. A partner can help with childcare, household responsibilities, and provide emotional support. Open communication and mutual understanding are key in managing postpartum depression and preventing further stress.
When to Seek Help
If you suspect that you or someone you know may be experiencing postpartum depression, it is crucial to seek help as soon as possible. While mild cases of “baby blues” typically resolve within two weeks, postpartum depression can persist for months if left untreated.
If you experience thoughts of harming yourself or your baby, contact a healthcare provider immediately or go to the nearest emergency room. It’s essential to act quickly to prevent further complications.
Conclusion
Postpartum depression is a common and serious mental health condition that can affect many new mothers. The symptoms of PPD can range from mild to severe, but the good news is that it is treatable. By recognizing the signs and seeking the appropriate treatment, mothers can overcome postpartum depression and regain their well-being. If you or someone you know is struggling with postpartum depression, know that help is available. Reach out to a healthcare provider, therapist, or support group to begin the journey toward recovery. Your mental health matters, and there is no shame in asking for help.

Exploring Antidepressants: How They Work and What You Need to Know
Antidepressants are among of the most often prescribed drugs for treating depression and other mental health issues. If you suffer from depression, anxiety, or another mood disorder, understanding how antidepressants work, as well as their possible benefits and side effects, is critical for making an informed treatment decision. In this article, we’ll look at what antidepressants are, how they function, and what you should know before using them as part of your treatment.
What are antidepressants?
Antidepressants are drugs that work by altering the chemistry of the brain to relieve symptoms of depression, anxiety, and other mood disorders. They function by modifying the levels of specific neurotransmitters in the brain, including as serotonin, norepinephrine, and dopamine, which play an important role in regulating mood.
How do antidepressants work?

The brain communicates using chemical signals, and neurotransmitters are the messengers that transport these signals between nerve cells. Depression can disturb the equilibrium of neurotransmitters, resulting in emotions of melancholy, hopelessness, and disinterest in daily activities. Antidepressants function by boosting the availability of these neurotransmitters or limiting their reabsorption, thereby restoring the brain’s normal chemical balance.
Antidepressants are classified into numerous kinds, which include:
Selective Serotonin Reuptake Inhibitors (SSRIs) are the most often prescribed antidepressants. They increase serotonin levels in the brain by inhibiting reabsorption.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): These medications affect both serotonin and norepinephrine levels, hence improving mood and reducing anxiety.
Tricyclic Antidepressants (TCAs): These older antidepressants function by inhibiting serotonin and norepinephrine reabsorption, although they have more adverse effects than SSRIs and SNRIs.
Monoamine Oxidase Inhibitors (MAOIs): These inhibit the breakdown of neurotransmitters and are commonly used when other antidepressants are ineffective.
What to Expect While Taking Antidepressants
When beginning antidepressant medication, it is critical to know that they do not provide immediate relief. Antidepressants can take 2 to 4 weeks to start working, and sometimes even longer to feel the full benefit. During this period, it is critical to maintain regular touch with your healthcare practitioner to discuss how you are feeling and whether your treatment plan needs to be adjusted.
Side Effects of Antidepressants
While antidepressants can be extremely helpful, they may cause negative effects. Common side effects could include:
- Nausea
- insomnia or sleepiness.
- Dry mouth.
- Weight changes.
- Sexual dysfunction.
- Increased anxiousness throughout the first few weeks of treatment.
Antidepressants can also trigger more serious adverse effects, such as suicidal ideation or self-harm, especially in young people. If you notice any unexpected mood swings or upsetting thoughts, seek quick help.
Finding the Right Antidepressant for You.
Not all antidepressants work the same for everyone. Before prescribing the appropriate prescription, your healthcare practitioner will carefully consider your symptoms, medical history, and other medications you are already taking. It is also usual for people to go through a trial-and-error phase, trying several antidepressants or modifying doses until they find the one that works best for them.
The Role of Therapy and Lifestyle Change

While antidepressants can be useful in treatment, they are frequently most effective when paired with psychotherapy, such as Cognitive Behavioral Therapy (CBT), and lifestyle changes such as regular exercise, a healthy diet, and decent sleeping habits. Addressing the underlying causes of depression via therapy and implementing healthy lifestyle changes can improve your overall mental health and lessen the need for long-term pharmaceutical use.
Conclusion
Antidepressants can be an effective tool for managing depression and improving mental health, but they are not a one-size-fits-all treatmenT. It is critical to work closely with your doctor to determine the best treatment for your specific condition and to be aware of any potential adverse effects.

The Promise of Ketamine in Treating Resistant Depression: A Breakthrough in Mental Health
Depression is one of the most common mental health disorders, affecting millions of people worldwide. While traditional treatments like antidepressants and psychotherapy work for many, a significant portion of individuals struggle with treatment-resistant depression (TRD). For these patients, finding relief can feel like an endless battle. Enter ketamine—a drug once known primarily as an anesthetic and, controversially, a recreational substance. Today, ketamine is gaining recognition as a groundbreaking treatment for resistant depression, offering hope to those who have exhausted other options. In this blog, we’ll explore the science behind ketamine, its benefits, potential risks, and what the future holds for this innovative therapy.
What is Treatment-Resistant Depression?
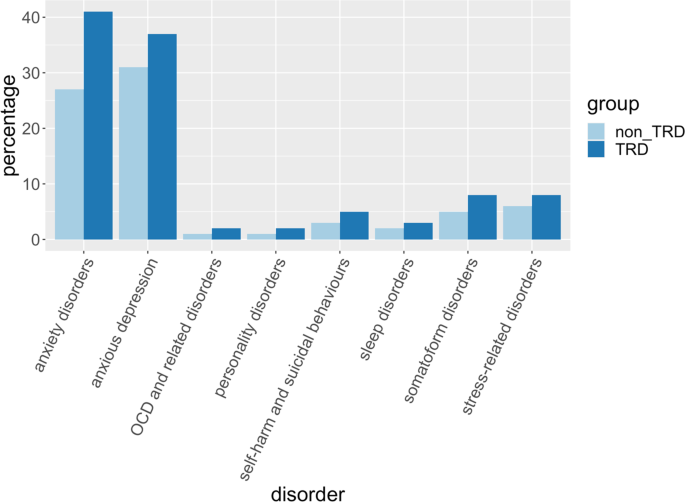
Treatment-resistant depression (TRD) is a severe form of depression that does not respond to standard treatments, such as selective serotonin reuptake inhibitors (SSRIs) or cognitive-behavioral therapy (CBT). Patients with TRD often experience persistent symptoms, including overwhelming sadness, fatigue, loss of interest in activities, and even suicidal thoughts, despite trying multiple medications and therapies. For these individuals, ketamine has emerged as a promising alternative.
What is Ketamine?
Ketamine is a dissociative anesthetic that has been used in medical settings since the 1960s, primarily for surgery and pain management. It works by blocking N-methyl-D-aspartate (NMDA) receptors in the brain, which play a role in mood regulation and synaptic plasticity. In recent years, researchers discovered that ketamine, when administered in low doses, can have rapid and profound antidepressant effects—often within hours or days, compared to weeks or months for traditional antidepressants.
How Does Ketamine Work for Depression?
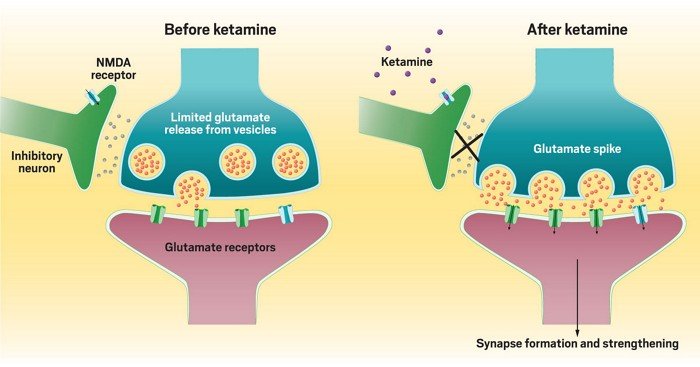
The exact mechanism of ketamine’s antidepressant effects is still being studied, but researchers believe it involves several key processes:
- NMDA Receptor Modulation: Ketamine blocks NMDA receptors, leading to increased production of glutamate, a neurotransmitter that enhances communication between brain cells. This boost in glutamate activity promotes the growth of new neural connections, which can help repair the brain’s damaged circuits associated with depression.
- Synaptic Plasticity: Ketamine stimulates the formation of new synapses (connections between neurons), which is crucial for learning, memory, and emotional regulation. This process may help “reset” the brain in individuals with depression.
- Rapid Relief: Unlike traditional antidepressants, which can take weeks to show effects, ketamine often provides relief within hours. This makes it particularly valuable for individuals experiencing severe depressive episodes or suicidal ideation.
- Anti-Inflammatory Effects: Emerging research suggests that depression may be linked to inflammation in the brain. Ketamine has been shown to reduce inflammatory markers, potentially contributing to its antidepressant effects.
The Benefits of Ketamine for Resistant Depression
Ketamine’s unique properties make it a game-changer for individuals with TRD. Here are some of its most notable benefits:
- Rapid Onset of Action: For patients in crisis, ketamine can provide relief within hours, offering a lifeline when traditional treatments fail.
- High Efficacy: Studies have shown that up to 70% of patients with TRD experience significant improvement after ketamine treatment, even when other therapies have not worked.
- Short-Term Treatment: Ketamine is typically administered in a series of infusions over a few weeks, making it a time-efficient option compared to long-term medication use.
- Reduced Suicidal Ideation: Ketamine has been shown to rapidly reduce suicidal thoughts, making it a critical tool for preventing suicide in high-risk individuals.
- Improved Quality of Life: Many patients report not only a reduction in depressive symptoms but also an overall improvement in their ability to function and enjoy life.
How is Ketamine Administered?
Ketamine for depression is typically administered in one of two ways:
- Intravenous (IV) Infusions: This is the most common and well-studied method. Patients receive a low dose of ketamine through an IV over 40 minutes to an hour, usually in a clinical setting. A series of 6-8 infusions over 2-3 weeks is often recommended for optimal results.
- Nasal Spray (Esketamine): In 2019, the FDA approved Spravato, a nasal spray containing esketamine (a derivative of ketamine), for treatment-resistant depression. It is used in conjunction with an oral antidepressant and is administered under medical supervision.
Other forms, such as oral tablets or intramuscular injections, are less common and not as widely studied.
Potential Risks and Side Effects
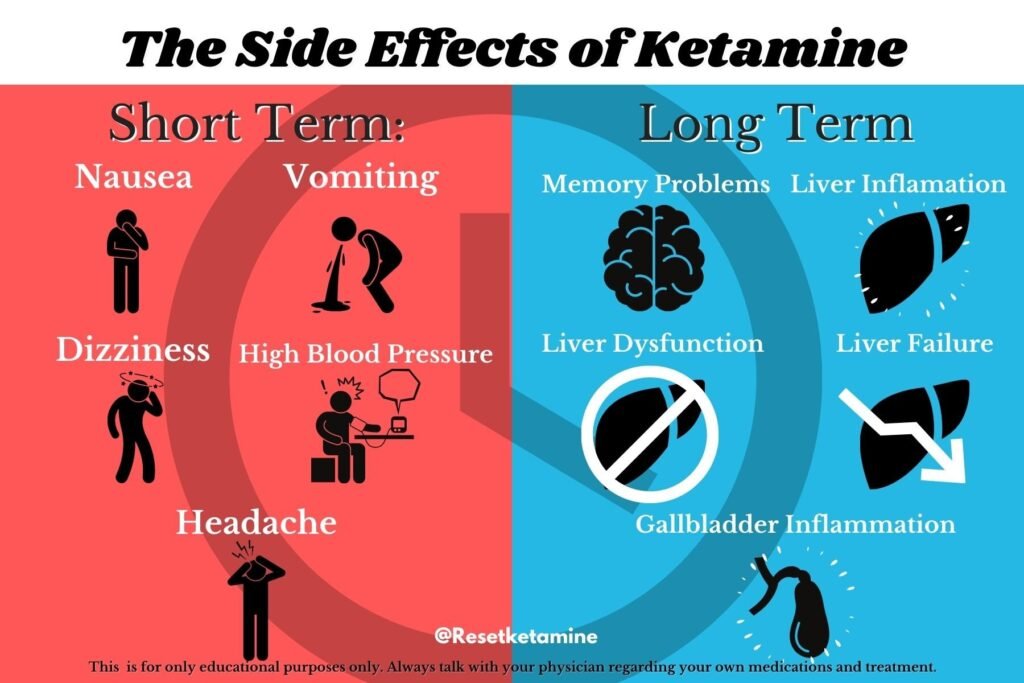
While ketamine offers significant promise, it is not without risks. Some potential side effects include:
- Dissociation: Patients may experience a temporary sense of detachment from reality during or shortly after treatment.
- Dizziness or Nausea: These are common but usually short-lived side effects.
- Increased Blood Pressure: Ketamine can cause a temporary rise in blood pressure, which is why it is administered under medical supervision.
- Potential for Abuse: Ketamine has a history of recreational use, so it is essential to use it only as prescribed and in a controlled setting.
Long-term effects of ketamine treatment are still being studied, and more research is needed to fully understand its safety profile.
Who is a Good Candidate for Ketamine Therapy?
Ketamine therapy is not a first-line treatment for depression. It is typically recommended for individuals who:
- Have not responded to at least two traditional antidepressant treatments.
- Are experiencing severe depressive symptoms or suicidal thoughts.
- Are under the care of a mental health professional who can monitor their progress.
It is not recommended for individuals with certain medical conditions, such as uncontrolled high blood pressure or a history of substance abuse, without careful evaluation.
The Future of Ketamine in Mental Health
The success of ketamine in treating resistant depression has sparked a wave of research into its potential applications for other mental health conditions, such as:
- Bipolar Disorder: Early studies suggest ketamine may help with depressive episodes in bipolar patients.
- Post-Traumatic Stress Disorder (PTSD): Ketamine’s ability to promote synaptic plasticity may help individuals process and recover from trauma.
- Chronic Pain Conditions: Ketamine’s pain-relieving properties are being explored for conditions like fibromyalgia and neuropathic pain.
Additionally, researchers are investigating ways to enhance ketamine’s benefits while minimizing its risks, such as developing new drugs that target the same pathways without the dissociative effects.
Conclusion
Ketamine represents a groundbreaking advancement in the treatment of resistant depression, offering hope to those who have struggled to find relief through traditional methods. Its rapid onset of action, high efficacy, and ability to reduce suicidal ideation make it a valuable tool in the mental health arsenal. However, it is not a one-size-fits-all solution, and its use must be carefully monitored by healthcare professionals.
If you or a loved one is struggling with treatment-resistant depression, ketamine therapy may be worth exploring. Consult with a mental health provider to determine if it is the right option for you. As research continues, the promise of ketamine and similar treatments offers a brighter future for individuals living with depression.
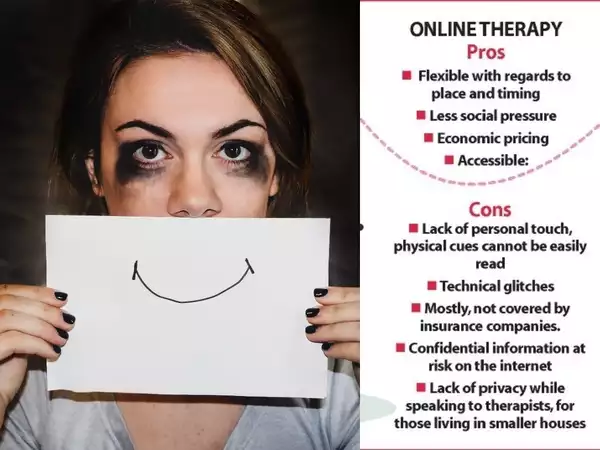
The Pros and Cons of Online Therapy for Anxiety
Anxiety disorders affect millions of people worldwide, making it one of the most common mental health concerns today. With the rise of digital health services, online therapy has become a popular alternative to traditional face-to-face counseling. But is online therapy effective for managing anxiety? In this blog, we’ll explore the pros and cons of online therapy for anxiety to help you determine if it’s the right choice for you.
Pros of Online Therapy for Anxiety

1. Accessibility and Convenience
One of the biggest advantages of online therapy is accessibility. Traditional therapy often requires travel, long waiting times, and limited availability of therapists in certain areas. With online therapy, you can connect with licensed professionals from the comfort of your home, eliminating the need for commuting and allowing therapy to fit into your schedule more easily.
2. Affordability
Many online therapy platforms offer more affordable options compared to in-person sessions. Without the costs associated with office rentals and commuting, therapists can charge lower fees. Additionally, many platforms provide subscription-based models, which can be more cost-effective than traditional hourly sessions.
3. Increased Privacy and Anonymity
For individuals struggling with anxiety, visiting a therapist’s office can feel intimidating. Online therapy offers a sense of privacy and anonymity, reducing the fear of being seen or judged. This can be especially beneficial for those with social anxiety who may find face-to-face interactions overwhelming.
4. Variety of Communication Options
Online therapy provides multiple ways to communicate, including video calls, phone calls, live chat, and even text messaging. This flexibility allows users to choose the format that feels most comfortable for them, making it easier to open up about their struggles with anxiety.
5. Access to a Wider Range of Therapists
When seeking traditional therapy, you are often limited to professionals within your geographical area. Online therapy platforms provide access to a diverse range of therapists with different specialties, allowing you to find a professional who best suits your needs.
6. Faster Appointment Scheduling
Finding a therapist with available appointments can be challenging, especially in high-demand areas. Online therapy platforms often have more availability, allowing you to schedule sessions more quickly and receive timely support when you need it the most.
7. Continuity of Care
For those who travel frequently or have unpredictable schedules, online therapy ensures continuity of care. You can continue your therapy sessions without interruption, regardless of your location.
Cons of Online Therapy for Anxiety

1. Limited Non-Verbal Communication
Non-verbal cues, such as body language and facial expressions, play a crucial role in traditional therapy sessions. In online therapy, especially through chat-based methods, therapists may miss these cues, making it harder to assess emotions accurately.
2. Technology Issues
Internet connectivity issues, poor video quality, or technical glitches can disrupt online therapy sessions. These issues can lead to frustration and impact the effectiveness of the session.
3. Not Suitable for Severe Anxiety or Crisis Situations
While online therapy is effective for mild to moderate anxiety, it may not be suitable for individuals experiencing severe anxiety disorders, suicidal thoughts, or psychiatric crises. In such cases, in-person therapy or immediate intervention from mental health professionals is recommended.
4. Insurance Coverage Limitations
Not all insurance providers cover online therapy, which can make it a less viable option for those relying on insurance benefits. It’s important to check with your insurance provider to understand your coverage options.
5. Risk of Unqualified Therapists
The rise of online therapy has also led to the emergence of unlicensed or unqualified practitioners. While many reputable platforms verify their therapists’ credentials, it’s essential to research and choose a legitimate service to ensure you receive professional care.
6. Less Personal Connection
Some individuals find that online therapy lacks the personal connection of face-to-face interactions. In-person sessions may provide a stronger therapeutic bond, which can be important for effective treatment.
7. Potential Security and Confidentiality Concerns
Although online therapy platforms use encryption and privacy measures, there is always a risk of data breaches. It’s crucial to choose a platform that prioritizes client confidentiality and follows strict security protocols.
Is Online Therapy Right for You?
The decision to pursue online therapy depends on your personal preferences, the severity of your anxiety, and your comfort with digital communication. If you value convenience, affordability, and privacy, online therapy may be a great option. However, if you require more intensive care, non-verbal communication, or crisis intervention, in-person therapy may be more suitable.
How to Choose the Best Online Therapy Platform
If you’re considering online therapy for anxiety, here are a few tips to help you choose the right platform:
- Check Therapist Credentials: Ensure the platform verifies the qualifications and licenses of its therapists.
- Read Reviews: Look for user feedback and testimonials to gauge the effectiveness of the service.
- Understand Pricing Plans: Compare subscription models and session fees to find an option that fits your budget.
- Verify Security Measures: Choose a platform that prioritizes data security and client confidentiality.
- Confirm Insurance Coverage: If you have insurance, check whether your provider covers online therapy sessions.
Conclusion
Online therapy is a convenient and effective option for managing anxiety, offering flexibility, affordability, and access to professional care from the comfort of your home. However, it’s important to weigh the pros and cons to determine if it aligns with your needs. If you’re struggling with anxiety, seeking help—whether online or in person—is a crucial step toward improving your mental well-being.
By making an informed decision, you can find the right therapy approach that supports your journey to a healthier and more balanced life.
What Causes PTSD? Exploring the Role of Trauma and Stress
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. While not everyone who experiences trauma develops PTSD, understanding the causes and risk factors can help shed light on why some individuals are more vulnerable than others. In this blog, we’ll explore what causes PTSD, focusing on the role of trauma, stress, and other contributing factors.
What Is PTSD?
PTSD is a mental health disorder characterized by intense, disturbing thoughts and feelings related to a traumatic event. Symptoms may include flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event. These symptoms can persist for months or even years, significantly impacting daily life.
While PTSD is often associated with veterans, it can affect anyone who has experienced trauma, such as survivors of abuse, accidents, natural disasters, or violent crimes.
The Role of Trauma in it
Trauma is the primary trigger for PTSD. However, not all traumatic events lead to this. The type, severity, and duration of the trauma play a significant role in whether someone develops the condition.
Types of Trauma Linked to it
- Combat and Military Trauma: Veterans and active-duty military personnel are at high risk due to exposure to life-threatening situations, violence, and the stress of war.
- Physical or Sexual Abuse: Survivors of abuse, whether in childhood or adulthood, often experience long-lasting psychological effects.
- Natural Disasters: Events like earthquakes, hurricanes, or floods can leave individuals feeling helpless and traumatized.
- Serious Accidents: Car crashes, workplace accidents, or other life-threatening incidents can trigger PTSD.
- Violent Crimes: Being a victim of or witnessing assault, robbery, or terrorism can lead to PTSD.
- Medical Trauma: Life-threatening illnesses, surgeries, or traumatic medical procedures can also be a cause.
Why Some Trauma Leads to it
Not everyone who experiences trauma develops PTSD. Factors that increase the likelihood include:
- The intensity and duration of the trauma.
- Feeling a lack of control during the event.
- The presence of physical injury or pain.
- A lack of social support after the event.
The Role of Stress in PTSD
Stress is a natural response to danger, but when it becomes chronic or overwhelming, it can contribute to the development of PTSD.
Acute Stress vs. Chronic Stress
- Acute Stress: This is the immediate reaction to a traumatic event, often referred to as the “fight or flight” response. For most people, these symptoms subside over time.
- Chronic Stress: When stress persists long after the traumatic event, it can disrupt the brain’s ability to process the experience, leading to PTSD.
How Stress Affects the Brain
PTSD is linked to changes in brain function, particularly in areas like the amygdala, hippocampus, and prefrontal cortex. These regions regulate fear, memory, and decision-making. Chronic stress can:
- Heighten Fear Responses: The amygdala becomes overactive, making individuals more sensitive to potential threats.
- Impair Memory Processing: The hippocampus, which helps process memories, may shrink, making it harder to distinguish between past and present.
- Reduce Emotional Regulation: The prefrontal cortex, responsible for rational thinking, may become less active, leading to difficulty managing emotions.
Risk Factors for Developing PTSD

While trauma and stress are the primary causes of PTSD, certain risk factors can increase susceptibility:
Biological Factors
- Genetics: A family history of anxiety or depression may increase the risk.
- Brain Chemistry: Imbalances in neurotransmitters like serotonin and dopamine can play a role.
- Hormonal Changes: Elevated levels of stress hormones like cortisol can contribute to PTSD.
Psychological Factors
- Previous Trauma: Individuals who have experienced trauma earlier in life are more vulnerable.
- Mental Health History: A history of anxiety, depression, or other mental health conditions can increase risk.
- Coping Mechanisms: Poor coping skills or a tendency to avoid problems can make it harder to process trauma.
Environmental Factors
- Lack of Social Support: A strong support system can help mitigate the effects of trauma.
- Ongoing Stress: Living in a high-stress environment can exacerbate symptoms.
- Childhood Adversity: Abuse, neglect, or unstable family environments during childhood can increase vulnerability.
Why Some People Don’t Develop PTSD
Resilience plays a significant role in why some individuals recover from trauma while others develop PTSD. Factors that contribute to resilience include:
- Strong Social Support: Having friends, family, or a community to lean on.
- Healthy Coping Mechanisms: Practices like mindfulness, exercise, or therapy.
- Positive Outlook: A sense of optimism and the ability to find meaning in adversity.
How Trauma and Stress Interact
Trauma and stress often work together to create the conditions for PTSD. For example:
- A traumatic event triggers an acute stress response.
- If the stress persists, it can lead to changes in brain function and chemistry.
- Without proper support or treatment, these changes can develop into PTSD.
Preventing PTSD After Trauma
While not all cases of PTSD can be prevented, early intervention can reduce the risk. Strategies include:
- Seeking Professional Help: Therapy, such as Cognitive Behavioral Therapy (CBT), can help process trauma.
- Building a Support Network: Connecting with loved ones or support groups can provide emotional relief.
- Practicing Self-Care: Exercise, healthy eating, and mindfulness can reduce stress levels.
- Avoiding Avoidance: Facing and processing emotions related to the trauma, rather than avoiding them, can prevent long-term issues.
Treatment Options for PTSD
If PTSD develops, effective treatments are available:
- Therapy: CBT, Eye Movement Desensitization and Reprocessing (EMDR), and exposure therapy are commonly used.
- Medication: Antidepressants or anti-anxiety medications can help manage symptoms.
- Lifestyle Changes: Regular exercise, a balanced diet, and stress management techniques can support recovery.
- Support Groups: Connecting with others who have experienced similar trauma can provide comfort and understanding.
Final Thoughts
PTSD is a complex condition rooted in the interplay between trauma, stress, and individual vulnerability. While not everyone who experiences trauma develops PTSD, understanding the causes and risk factors can help individuals seek timely support and treatment. If you or someone you know is struggling with PTSD, remember that help is available, and recovery is possible.
By raising awareness and fostering understanding, we can create a more supportive environment for those affected by PTSD. If you found this blog helpful, share it with someone who might benefit, and let us know your thoughts in the comments below.
10 Effective Ways to Calm an Anxiety Attack in the Moment
Anxiety attacks can feel overwhelming, leaving you breathless, panicked, and out of control. Whether you’ve experienced them before or are facing one for the first time, knowing how to calm yourself in the moment can make a world of difference. In this blog, we’ll explore 10 effective ways to calm an anxiety attack, offering practical, actionable strategies to help you regain control and find relief.
What Is an Anxiety Attack?

An anxiety attack, often confused with a panic attack, is a sudden episode of intense fear or discomfort. Symptoms may include rapid heartbeat, shortness of breath, sweating, trembling, and a sense of impending doom. While anxiety attacks can be terrifying, they are not life-threatening, and there are proven techniques to manage them.
1. Practice Deep Breathing
When anxiety strikes, your breathing often becomes shallow and rapid, which can worsen symptoms. Deep breathing helps activate your body’s relaxation response.
- How to Do It: Sit or lie down in a comfortable position. Place one hand on your chest and the other on your stomach. Inhale slowly through your nose for a count of four, hold for four seconds, and exhale through your mouth for a count of six. Repeat until you feel calmer.
- Why It Works: Deep breathing slows your heart rate and signals your brain to relax.
2. Use Grounding Techniques
Grounding techniques help you reconnect with the present moment, pulling your focus away from anxious thoughts.
- 5-4-3-2-1 Method: Identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste. This sensory exercise anchors you in the present.
- Why It Works: Grounding distracts your mind from spiraling thoughts and brings you back to reality.
3. Try Progressive Muscle Relaxation

Progressive muscle relaxation (PMR) involves tensing and then relaxing different muscle groups to release physical tension.
- How to Do It: Start with your toes. Tense the muscles for five seconds, then release. Move upward to your calves, thighs, abdomen, arms, and face.
- Why It Works: PMR reduces physical tension, which can help alleviate the physical symptoms of anxiety.
4. Focus on a Mantra or Affirmation
Repeating a calming phrase can help shift your mindset during an anxiety attack.
- Examples: “This too shall pass,” “I am safe,” or “I can handle this.”
- Why It Works: Mantras provide a mental anchor, helping you focus on positivity rather than fear.
5. Engage Your Senses
Engaging your senses can help distract your mind and calm your body.
- Try This: Hold a piece of ice, smell lavender oil, listen to calming music, or sip a warm drink.
- Why It Works: Sensory input can interrupt the anxiety cycle and provide immediate relief.
6. Practice Visualization
Visualization involves imagining a peaceful scene to distract your mind from anxiety.
- How to Do It: Close your eyes and picture a place where you feel safe and relaxed, such as a beach or forest. Imagine the sights, sounds, and smells of this place.
- Why It Works: Visualization shifts your focus away from anxiety and promotes relaxation.
7. Use the “3-3-3 Rule”
The 3-3-3 rule is a simple grounding technique to refocus your mind.
- How to Do It: Name three things you can see, three sounds you can hear, and move three parts of your body (e.g., wiggle your toes, shrug your shoulders, nod your head).
- Why It Works: This technique helps you reconnect with your surroundings and break the cycle of anxious thoughts.
8. Reach Out to Someone You Trust
Talking to someone you trust can provide immediate comfort and reassurance.
- What to Do: Call or text a friend, family member, or therapist. Simply saying, “I’m having an anxiety attack” can help you feel less alone.
- Why It Works: Social support can reduce feelings of isolation and provide a sense of safety.
9. Move Your Body
Physical activity can help release pent-up energy and reduce anxiety symptoms.
- Try This: Go for a walk, stretch, or do light yoga. Even shaking out your hands or jumping in place can help.
- Why It Works: Movement releases endorphins, which are natural mood boosters, and helps regulate your nervous system.
10. Practice Self-Compassion
During an anxiety attack, it’s easy to be hard on yourself. Practicing self-compassion can help you navigate the experience with kindness.
- What to Do: Remind yourself that anxiety attacks are temporary and that you’re doing your best. Say to yourself, “It’s okay to feel this way. I will get through this.”
- Why It Works: Self-compassion reduces shame and helps you approach the situation with a calmer mindset.
Preventing Future Anxiety Attacks
While these techniques can help in the moment, it’s also important to address the root causes of anxiety. Consider:
- Therapy: Cognitive Behavioral Therapy (CBT) is highly effective for managing anxiety.
- Lifestyle Changes: Regular exercise, a balanced diet, and adequate sleep can reduce anxiety over time.
- Mindfulness Practices: Meditation, yoga, and journaling can help you build resilience against anxiety.
When to Seek Professional Help
If anxiety attacks are frequent, severe, or interfering with your daily life, it’s important to seek professional help. A therapist or doctor can provide personalized treatment options, such as therapy, medication, or a combination of both.
Final Thoughts
Anxiety attacks can feel overwhelming, but with the right tools, you can regain control and find relief. By practicing deep breathing, grounding techniques, and self-compassion, you can calm your mind and body during an anxiety attack. Remember, you’re not alone, and help is always available.
If you found this blog helpful, share it with someone who might benefit, and let us know your favorite anxiety-relief techniques in the comments below!
