
The Promise of Ketamine in Treating Resistant Depression: A Breakthrough in Mental Health
Depression is one of the most common mental health disorders, affecting millions of people worldwide. While traditional treatments like antidepressants and psychotherapy work for many, a significant portion of individuals struggle with treatment-resistant depression (TRD). For these patients, finding relief can feel like an endless battle. Enter ketamine—a drug once known primarily as an anesthetic and, controversially, a recreational substance. Today, ketamine is gaining recognition as a groundbreaking treatment for resistant depression, offering hope to those who have exhausted other options. In this blog, we’ll explore the science behind ketamine, its benefits, potential risks, and what the future holds for this innovative therapy.
What is Treatment-Resistant Depression?
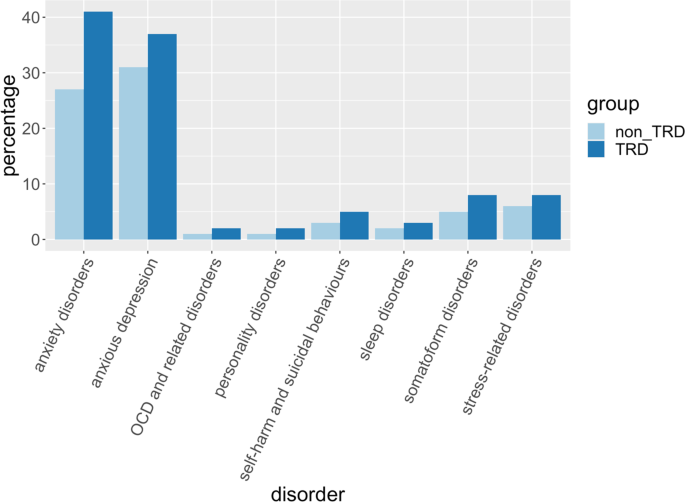
Treatment-resistant depression (TRD) is a severe form of depression that does not respond to standard treatments, such as selective serotonin reuptake inhibitors (SSRIs) or cognitive-behavioral therapy (CBT). Patients with TRD often experience persistent symptoms, including overwhelming sadness, fatigue, loss of interest in activities, and even suicidal thoughts, despite trying multiple medications and therapies. For these individuals, ketamine has emerged as a promising alternative.
What is Ketamine?
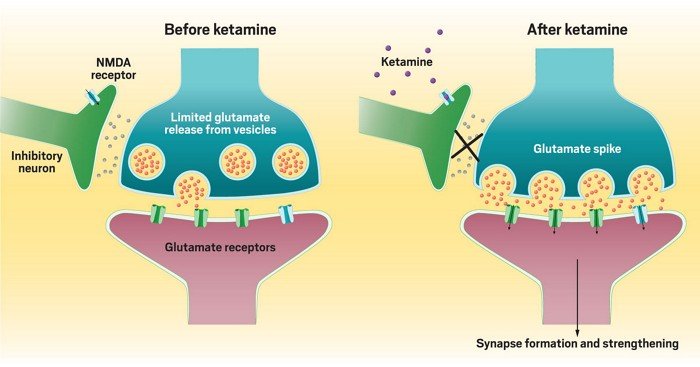
Ketamine is a dissociative anesthetic that has been used in medical settings since the 1960s, primarily for surgery and pain management. It works by blocking N-methyl-D-aspartate (NMDA) receptors in the brain, which play a role in mood regulation and synaptic plasticity. In recent years, researchers discovered that ketamine, when administered in low doses, can have rapid and profound antidepressant effects—often within hours or days, compared to weeks or months for traditional antidepressants.
How Does Ketamine Work for Depression?
The exact mechanism of ketamine’s antidepressant effects is still being studied, but researchers believe it involves several key processes:
- NMDA Receptor Modulation: Ketamine blocks NMDA receptors, leading to increased production of glutamate, a neurotransmitter that enhances communication between brain cells. This boost in glutamate activity promotes the growth of new neural connections, which can help repair the brain’s damaged circuits associated with depression.
- Synaptic Plasticity: Ketamine stimulates the formation of new synapses (connections between neurons), which is crucial for learning, memory, and emotional regulation. This process may help “reset” the brain in individuals with depression.
- Rapid Relief: Unlike traditional antidepressants, which can take weeks to show effects, ketamine often provides relief within hours. This makes it particularly valuable for individuals experiencing severe depressive episodes or suicidal ideation.
- Anti-Inflammatory Effects: Emerging research suggests that depression may be linked to inflammation in the brain. Ketamine has been shown to reduce inflammatory markers, potentially contributing to its antidepressant effects.
The Benefits of Ketamine for Resistant Depression
Ketamine’s unique properties make it a game-changer for individuals with TRD. Here are some of its most notable benefits:
- Rapid Onset of Action: For patients in crisis, ketamine can provide relief within hours, offering a lifeline when traditional treatments fail.
- High Efficacy: Studies have shown that up to 70% of patients with TRD experience significant improvement after ketamine treatment, even when other therapies have not worked.
- Short-Term Treatment: Ketamine is typically administered in a series of infusions over a few weeks, making it a time-efficient option compared to long-term medication use.
- Reduced Suicidal Ideation: Ketamine has been shown to rapidly reduce suicidal thoughts, making it a critical tool for preventing suicide in high-risk individuals.
- Improved Quality of Life: Many patients report not only a reduction in depressive symptoms but also an overall improvement in their ability to function and enjoy life.
How is Ketamine Administered?
Ketamine for depression is typically administered in one of two ways:
- Intravenous (IV) Infusions: This is the most common and well-studied method. Patients receive a low dose of ketamine through an IV over 40 minutes to an hour, usually in a clinical setting. A series of 6-8 infusions over 2-3 weeks is often recommended for optimal results.
- Nasal Spray (Esketamine): In 2019, the FDA approved Spravato, a nasal spray containing esketamine (a derivative of ketamine), for treatment-resistant depression. It is used in conjunction with an oral antidepressant and is administered under medical supervision.
Other forms, such as oral tablets or intramuscular injections, are less common and not as widely studied.
Potential Risks and Side Effects
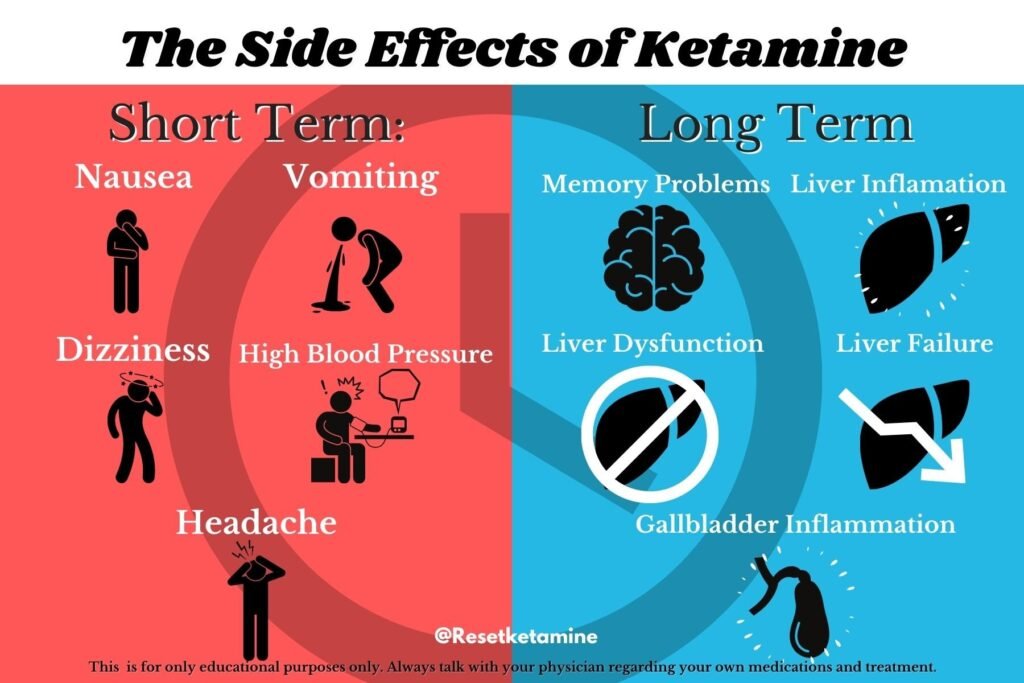
While ketamine offers significant promise, it is not without risks. Some potential side effects include:
- Dissociation: Patients may experience a temporary sense of detachment from reality during or shortly after treatment.
- Dizziness or Nausea: These are common but usually short-lived side effects.
- Increased Blood Pressure: Ketamine can cause a temporary rise in blood pressure, which is why it is administered under medical supervision.
- Potential for Abuse: Ketamine has a history of recreational use, so it is essential to use it only as prescribed and in a controlled setting.
Long-term effects of ketamine treatment are still being studied, and more research is needed to fully understand its safety profile.
Who is a Good Candidate for Ketamine Therapy?
Ketamine therapy is not a first-line treatment for depression. It is typically recommended for individuals who:
- Have not responded to at least two traditional antidepressant treatments.
- Are experiencing severe depressive symptoms or suicidal thoughts.
- Are under the care of a mental health professional who can monitor their progress.
It is not recommended for individuals with certain medical conditions, such as uncontrolled high blood pressure or a history of substance abuse, without careful evaluation.
The Future of Ketamine in Mental Health
The success of ketamine in treating resistant depression has sparked a wave of research into its potential applications for other mental health conditions, such as:
- Bipolar Disorder: Early studies suggest ketamine may help with depressive episodes in bipolar patients.
- Post-Traumatic Stress Disorder (PTSD): Ketamine’s ability to promote synaptic plasticity may help individuals process and recover from trauma.
- Chronic Pain Conditions: Ketamine’s pain-relieving properties are being explored for conditions like fibromyalgia and neuropathic pain.
Additionally, researchers are investigating ways to enhance ketamine’s benefits while minimizing its risks, such as developing new drugs that target the same pathways without the dissociative effects.
Conclusion
Ketamine represents a groundbreaking advancement in the treatment of resistant depression, offering hope to those who have struggled to find relief through traditional methods. Its rapid onset of action, high efficacy, and ability to reduce suicidal ideation make it a valuable tool in the mental health arsenal. However, it is not a one-size-fits-all solution, and its use must be carefully monitored by healthcare professionals.
If you or a loved one is struggling with treatment-resistant depression, ketamine therapy may be worth exploring. Consult with a mental health provider to determine if it is the right option for you. As research continues, the promise of ketamine and similar treatments offers a brighter future for individuals living with depression.
